This guest post is presented by Maximus, sponsor of APHA’s Annual Meeting Blog. Its Center for Health Innovation offers programs and services to help governments respond to population health needs and emerging public health threats and improve public health infrastructure.
The Maximus Public Health team is working to improve information systems. Corinna Dan, RN, MPH, Maximus vice president, offers recommendations from the team to empower health departments to become self-reliant and use eCR, or electronic case reporting, which is an automated, real-time transmission of case report information between electronic health records and public health agencies.
COVID-19 revealed the weaknesses of the public health data ecosystem and provided evidence of the critical need to prioritize data modernization. Experts agree that public health data systems need major advances. But for state and local health departments, the task is enormous.
One area of growing importance in public health data modernization activities is electronic case reports, or eCRs. A relatively new and complex data stream, eCRs move data quickly and securely from electronic health records in health care facilities to state and local public health agencies. Implementing an eCR feed requires a collaborative process across health care providers and public health professionals.
eCR data is of higher volume and greater complexity than other data sources that public health receives, requiring new strategies for health departments. However, this data also holds great promise and ultimately will increase the timeliness and accuracy of public health data, improve data analytics, and reduce the burden of case investigation for overworked disease investigative specialists and epidemiologists.
How eCR works
An eCR is initiated when certain types of information are entered into the electronic health record. When any reportable or possibly reportable health condition diagnosis code is entered into a health record, an electronic transmission is triggered, sending an automated message to a health department. Health departments receive information about conditions that are reportable in their jurisdiction only through a centralized tool called the Reportable Conditions Knowledge Management System.
Compared to the ways in which reportable case data has been sent historically — through mail, fax or online using a dedicated portal — eCR data is shared quickly and requires no additional data entry.
But the data is not in the brief case reporting format that health departments are familiar with. Rather, it is transmitted in a clinical format that needs to be adapted for public health use. This presents many challenges for public health data systems.
Current challenges
• High volumes of data: eCR data is sent each time a relevant trigger is added to a patient record, so health departments often receive multiple eCRs for a single patient in a single day. In addition, there is a short delay, about one hour, before sending to allow time for the clinical data from the health care visit to be captured.
The electronic health record periodically reviews all the recent eCRs sent — e.g., 12 hours following the initial trigger code — to check if new data is found and 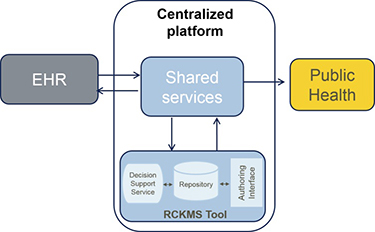 transmits that data again if a new code is identified. This review-and-transmit function continues for 72 hours after the initial event, so health departments continue to receive updated data on reportable conditions identified in health care settings.
transmits that data again if a new code is identified. This review-and-transmit function continues for 72 hours after the initial event, so health departments continue to receive updated data on reportable conditions identified in health care settings.
• Complex clinical data from electronic health records: The eCR comes directly from the clinical encounter data, so there are necessary steps to filter out old and unneeded data, identify and ingest the new data, and send it to the correct corresponding field in the public health data system. Several factors complicate this.
First, the electronic health records data are heterogeneous, because different health systems use different health records and customize the technology’s capabilities. Even when using the same records, various health care providers enter data differently.
The same clinical information is often put in different places in the health records, meaning the information can be in different or multiple locations in the eCR message. For example, one could find information about pregnancy in multiple areas — in the lab, diagnosis and social history sections. Codes from different health records are often different. Each health department will receive eCR data from multiple health records and health care organizations. The work must be coordinated between clinical and public health systems.
Second, there are often many ways to describe symptoms and conditions within medical terminology. This introduces additional complexity. For example, abdominal pain can be documented with further details about the location of the pain — right/left, upper/lower quadrant pain — or based on the cause of pain, such as severe abdominal cramping or stomach ache.
Third, data quality is low with many duplicate records causing additional challenges in transforming clinical data into public health case report data. Many providers do not have adequate time to ask all questions related to a condition and often mark “unknown” to save time. Most electronic health records contain data collected from each patient over multiple visits, so eCR ingestion must be able to identify relevant information about the new reportable condition.
Multiple versions of the same reportable condition are sent with changes over time as new information is added, requiring processes to identify the most appropriate data to use in the public health case report and then retain it in the public health data system.
• Non-interoperable, disconnected data systems: Clinical and public health data systems have very different types of data and data systems, despite both containing personal health information. Most jurisdictions use surveillance platforms established well before electronic health records were developed, and these systems are not set up to accept such complex data.
Changing data from an eCR format into the existing fields of a public health system takes a lot of effort. While in the past public health departments have undergone similar ingestion mapping exercises with the introduction of electronic lab reporting, these reports tend to be less duplicative and complex than eCRs.
Solutions exist
Public health data systems must evolve by using newly available data such as eCRs to improve data quality.
eCR ingestion holds the potential to improve data interoperability and quality without increasing the workload for staff. This new data source, currently being implemented across health systems because of new CMS regulations, provides access to data that supports public health’s role in emergency preparedness and response, increasing situational awareness and timely alerts related to reportable conditions such as Ebola and measles. These will, in turn, enable rapid response and mitigation measures to protect the health of the public.
Unfortunately, eCR ingestion and mapping likely seem insurmountable to many health departments because these tasks require significant data infrastructure to support large volumes of data as well as staff education and training on implementing and maintaining the system.
Maximus delivers state-of-the-art integrated services with hands-on experience in eCR implementation. Its public health services meet health departments where they are in their data modernization journey, from assessing current systems and planning a modernization roadmap to expanding interoperability by integrating new data sources, such as eCRs, and implementing data standards, such as HL7 and FHIR.
Top photo, courtesy Maximus.
Photo caption bottom: The Reportable Condition Knowledge Management System is an integral piece of the eCR centralized infrastructure. Public health agencies populate the tool with jurisdiction-reporting requirements so that electronic initial case reports from health care can be processed against them to determine if the case report is reportable and to which health agency the report should be sent. Photo courtesy Council of State and Territorial Epidemiologists, Reportable Conditions Knowledge Management and eCR.